Economics and Behavioral Health
Behavioral health disorders include serious mental illness and substance use disorders. These conditions are costly both to affected individuals and to society. Individuals with behavioral health disorders experience interpersonal problems, employment difficulties, reduced overall health, and increased risk of death. Behavioral health disorders can complicate general health treatment. These conditions are costly to society because they place demands on the criminal justice, social service, and health-care systems, and because they reduce labor market productivity. Behavioral health conditions cost the US economy more than $1 trillion each year.1 2 The causes of these disorders are complex, and likely include both genetic and environmental factors.
Behavioral health disorders are relatively common. The most recent government data suggest that, in 2017, 4.2 percent of all US adults — 11.2 million people — met diagnostic criteria for serious mental illness, and 7.2 percent — 19.2 million people — had substance abuse disorders. Approximately 1 percent — 3.1 million Americans — met criteria for both disorders.3 A much larger share of the population engages in misuse of substances through activities such as binge drinking and recreational use of drugs, or experiences episodes of poor mental health such as mild depression or anxiety. The United States is in the midst of an unprecedented drug-use epidemic.
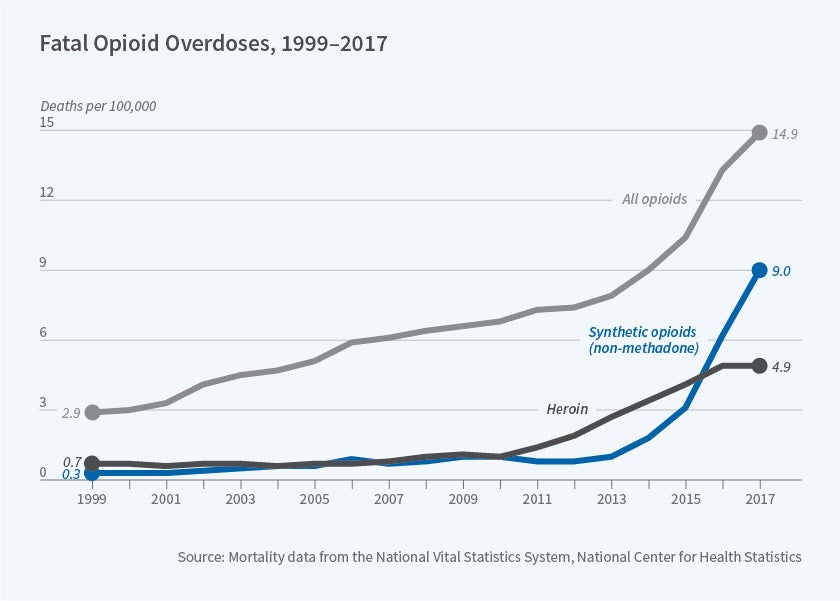
In 2017, 70,237 US residents are known to have died from a drug overdose. The drug-use epidemic has been largely attributable to opioids. There are 130 opioid-related overdose deaths each day, a rate that has increased more than sixfold since 1999.4 The opioid epidemic is believed to have begun in the 1990s and 2000s through overprescription of opioids for the treatment of pain. It has evolved over time to involve heroin and synthetic opioids.5 Abby Alpert, David Powell, and Rosalie Pacula, along with William Evans, Ethan Lieber, and Patrick Power, have documented that an unexpected, to consumers, reformulation of OxyContin in 2010, which limited the ability to abuse this then-most commonly used prescription opioid, led many users to transition to heroin and, more recently, to fentanyl and other synthetic opioids.6,7 Synthetic opioids are less expensive to manufacture but are more potent than heroin and prescription opioids. Figure 1 documents trends in annual overdoses associated with any opioid, heroin, and synthetic opioids (other than methadone, which is a medication used to treat opioid use disorder). The sharp uptick in the later period is ascribed to fentanyl in particular. Federal, state, and local governments have adopted a range of policies to address the opioid epidemic: prescription drug monitoring programs, shutdowns of "pill mills," a crackdown on doctor-shopping, syringe exchanges, and funds to support treatment.
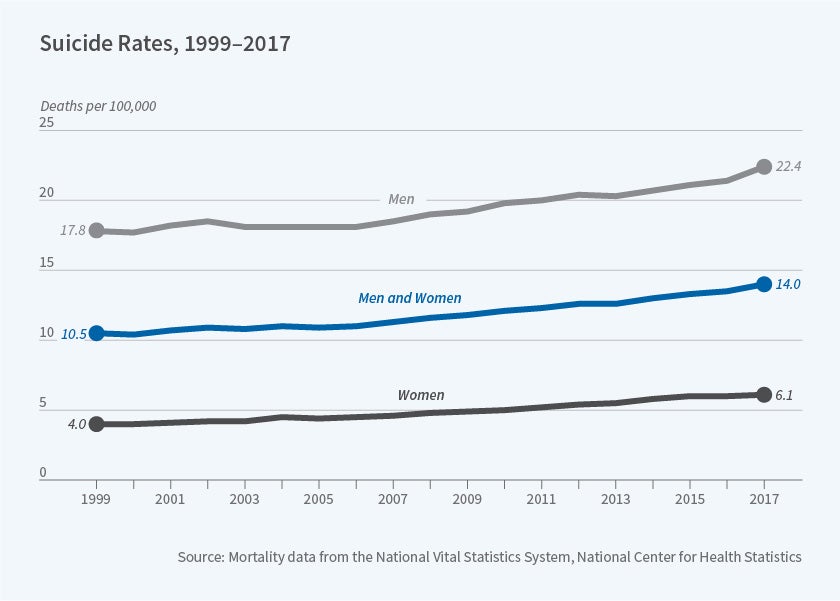
At the same time as the country is facing social costs from escalating drug misuse, government data suggest that suicide rates are also increasing. The overall rate and rates for men and women from 1999 through 2017 are shown in Figure 2. While behavioral health disorders generally cannot be cured, there is substantial medical evidence that these disorders can be managed. This confluence of factors creates an important potential role for public policy, which can provide insurance coverage that is sufficiently generous, in terms of covered benefits, to allow appropriate treatment. In a series of studies, my colleagues and I explore how insurance expansions can influence behavioral health-care service use and associated outcomes. To study these questions, we combine insight from health economics with clinical knowledge of behavioral health disorders. Both are important for studying these questions. We rely heavily on survey and administrative datasets maintained by the US government specifically to track behavioral health outcomes.
An important feature of the behavioral health-care delivery system, in particular the substance use disorder (SUD) system, is limited use of insurance payments. Many providers operate outside insurance payments, for example, accepting self-payments or relying on government grants and contracts to support treatment. Combining this feature with unique challenges faced by those with behavioral health disorders, such as stigma, makes the extent to which expanding insurance leads to changes in outcomes is an empirical question.
Evidence from Public Markets
Medicaid, which finances health-care services for low-income people, is the largest purchaser of US behavioral health care.8 Brendan Saloner and I examine the effect of Affordable Care Act (ACA) Medicaid expansions on SUD treatment, specialty treatment, and medications obtained in non-specialty settings such as physicians' offices.9 Medicaid-enrolled adults have elevated need for behavioral health-care treatment and are less likely to receive this modality of care than privately and Medicare-insured adults. The ACA reflects a major transformation of many areas of the health-care system. Pre-ACA, experts asserted that "no illness will be more affected than substance use disorders."10 We find that ACA-Medicaid expansion increased Medicaid coverage among patients receiving specialty care, and use of Medicaid to pay for treatment. Given the limited use of insurance within the SUD treatment delivery system, this latter finding is important; ACA-Medicaid allowed low-income adults with SUDs to enroll in Medicaid, and providers were able to accept that insurance as a form of payment. Our effect sizes are quite large, suggesting that when new forms of financing are available, patients and providers are elastic in their responses. We do not observe changes in admissions; we hypothesize that capacity constraints within the SUD treatment delivery system may have stifled effects in the short run, as we examine the situation two years post-expansion. In continuing research, we are exploring the longer-run effects, using data from four years post-expansion, and we observe increases in admissions, which is in line with our hypothesis. When we consider prescriptions for medications financed by Medicaid used to treat SUDs in office-based settings, a setting generally preferred by patients, we observe large increases in treatment uptake.
In terms of serious mental illness, Michael Pesko, Benjamin Cook, Nicholas Carson, and I show that ACA-Medicaid expansions increase use of prescriptions used to treat mental illness in office-based settings.11 Similarly, Elson Blunt, Ioana Popovici, Steven Marcus, and I use data on the universe of specialty mental health-care providers to study ACA-Medicaid effects.12 We show that following ACA-Medicaid expansion specialty providers are more likely to accept Medicaid as a form of payment, suggesting that this expansion is making new treatment options available to lower-income adults.
Sebastian Tello-Trillo, Douglas Webber, and I examine the effect of losing public insurance on hospitalizations for behavioral health-care outcomes.13 We exploit a large-scale and unexpected Medicaid disenrollment that occurred in the state of Tennessee in 2005 (TennCare). This disenrollment led to 190,000 low-income adults losing coverage that had included a generous set of behavioral health-care services. We show that losing TennCare reduced the number of SUD-related hospitalizations, while the number of mental illness hospitalizations was unchanged. Patients with mental illness were able to replace Medicaid with private and Medicare coverage, while patients with SUDs were not able to fill in the Medicaid gap and instead had to self-finance hospitalizations after the disenrollment. We hypothesize that patients with SUDs face important social, economic, and cognitive challenges that limit their ability to find substitute coverage following an insurance loss. We also show that, post-disenrollment, behavioral health outcomes decline, plausibly through reduced treatment for SUDs and other changes, such as increased financial strain, as has been shown by Laura Argys et al.14
Evidence from Private Markets
State governments have attempted to increase coverage of behavioral health-care services in private insurance contracts. Beginning in the 1970s, states have required either that private insurers include a minimum set of SUD treatment benefits in contracts or that the insurer offer a beneficiary the ability to include SUD treatment services. Even after adoption of these early mandates, coverage was relatively sparse and insurers could impose cost-sharing and service limitations that were more restrictive than those applied to general health-care services. Not until the mid-1990s did states begin to implement legislation that required coverage of SUD treatment services in private insurance contracts and equality between SUD and general health care services (parity laws).
Popovici, Elisheva Stern, and I study the effects of parity laws on specialty SUD treatment provider behavior.15 We show that following passage of a parity law, SUD treatment providers are more likely to accept private coverage and less likely to accept public coverage, and they increase the quantity of health care delivered. Provision of charity care declines post-parity law; we hypothesize that substitution effects — treating higher reimbursement-rate patients — crowds out care provided for free. Michael French, Popovici, and I consider the effects of parity law passage on a more distal outcome — substance-involved traffic fatalities. We show, using a range of administrative datasets, that following passage of a parity law, SUD treatment uptake increases, SUDs decline, and substance-involved traffic fatalities drop.16
An early provision of the ACA, the dependent coverage mandate (DCM) implemented in 2010, allowed many young adults to remain on their parents' private plan through age 26. The age limit previously was 19. Saloner, Cook, Yaa Akosa Antwi, and I examine the effect of the DCM on insurance coverage, payment forms, and admissions within the specialty sector.17 We compare trends in these outcomes for adults aged 20 to 26 to slightly older adults unaffected by the DCM. Similar to ACA-Medicaid, we observe large increases in private coverage and use of this insurance to pay for treatment within the target group. Interestingly, we observe a decline in admissions post-DCM. We hypothesize that the DCM allows young adults to receive care in other, perhaps more desirable, settings such as physicians' offices, rather than in the specialty settings that we examine. This is potentially important, as patients are more likely to remain in treatment, and therefore better manage their chronic condition, in settings that they find acceptable.
The Massachusetts Experience
The Massachusetts health-care reform of 2006 is viewed by many policy experts as the blueprint for the ACA. Both reforms aimed to achieve universal insurance through expansions of public and private coverage. Saloner and I leverage the Massachusetts experience to study how a large-scale insurance expansion in both the public and private markets might influence specialty SUD treatment.18 Massachusetts compelled private insurers to provide a relatively generous set of SUD treatment services, and Medicaid covered these services. We find no evidence that this reform led to changes in the number of admissions to treatment or in the types of payment that providers were willing to accept. Massachusetts is unique in that this state had one of the lowest uninsured rates in the country prior to its reform, thus our null findings may reflect ceiling effects.
Lessons Learned
Our findings are heterogeneous; there does not appear to be a "one size fits all" policy for addressing behavioral health issues. The effects of expanding coverage are much more nuanced and appear to depend on the affected population, treatment setting, and outcome. The mixed findings suggest that, while there is promise in using insurance policies to improve behavioral health, decision-makers must carefully assess the context in which a policy change is being considered.
Endnotes
"Societal Burden of Substance Abuse," Caulkins J, Kasunic A, Lee M. International Public Health Journal 6(3), 2014, pp. 269–282.
"Assessing the Economic Costs of Serious Mental Illness," Insel T. American Journal of Psychiatry 165(6), June 2008, pp. 663–665.
Key Substance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health," Bose J, Hedden S, Lipari R, Park-Lee E. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD, 2018.
"Drug Overdose Deaths in the United States, 1999–2017," Hedegaard H, Miniño A, Warner M. NCHS Data Brief 329, November 2018, National Center for Health Statistics.
Vietnam War Casualties (1955–1975). Military Factory, 2019.
"Supply-Side Drug Policy in the Presence of Substitutes: Evidence from the Introduction of Abuse-Deterrent Opioids," Alpert A, Powell D, Pacula R, NBER Working Paper 23031, January 2017, and American Economic Journal: Economic Policy 10(4), November 2018, pp. 1–35.
"How the Reformulation of OxyContin Ignited the Heroin Epidemic," Evans W, Lieber E, Power P. NBER Working Paper 24475, April 2018, and Review of Economics and Statistics 101(1), March 2019, pp. 1–15.
"Behavioral Health in the Medicaid Program — People, Use, and Expenditures," Medicaid and CHIP Payment and Access Commission, Washington, DC, June 2015.
"The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act," Maclean J, Saloner B. Journal of Policy Analysis and Management 38(2), Spring 2019, pp. 366–393.
"The Affordable Care Act and Treatment for 'Substance Use Disorders:' Implications of Ending Segregated Behavioral Health Care," McLellan A, Woodworth A. Journal of Substance Abuse Treatment 46(5), May-June 2014; pp. 541–545.
"Public Insurance and Psychotropic Prescription Medications for Mental Illness," Maclean J, Cook B, Carson J, Pesko M. NBER Working Paper 23760, March 2018, and B.E. Journal of Economics and Policy Analysis, 19(1), January 2019.
"Public Insurance Expansions and Mental Healthcare Availability," Blunt E, Maclean J, Popovici I, Marcus S. Working paper in progress.
"Losing Insurance and Behavioral Health Inpatient Care: Evidence from a large-scale Medicaid Disenrollment," Maclean J, Tello-Trillo S, Webber D. NBER Working Paper 25936, June 2019.
"Losing Public Health Insurance: TennCare Disenrollment and Personal Financial Distress," Argys L, Friedson A, Pitts M, Tello-Trillo S. Federal Reserve Bank of Atlanta Working Paper Series. Federal Reserve Bank of Atlanta, 2017.
"Health Insurance Expansions and Providers' Behavior: Evidence from Substance-Use-Disorder Treatment Providers," Maclean J, Popovici I, Stern E. Journal of Law & Economics 61(2), 2018, pp. 279–310.
"Health Insurance and Traffic Fatalities: The Effects of Substance Use Disorder Parity Laws," Popovici I, Maclean J, French M. NBER Working Paper 23388, February 2018.
"Access to Health Insurance and Utilization of Substance Use Disorder Treatment: Evidence from the Affordable Care Act Dependent Coverage Provision," Saloner B, Akosa Antwi Y, Maclean J, Cook B. Health Economics 27(1), January 2017, pp. 50–75.
"Substance Use Treatment Provider Behavior and Healthcare Reform: Evidence from Massachusetts," Maclean J, Saloner B. Health Economics 27(1), 2018, pp. 76–101.