Oregon Health Insurance Experiment - Results
Health Care Utilization
Using both administrative data and surveys, we found that in the first one to two years of coverage, Medicaid increased utilization of many different kinds of care, including outpatient care, prescription drugs, hospitalizations, and emergency department visits.
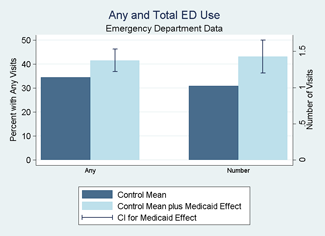
Emergency Department Visits
- Using emergency department records from Portland-area hospitals, we found that Medicaid coverage substantially increased emergency department use.
- Medicaid increased the probability of using the emergency department by 7 percentage points (an increase of about 20 percent, relative to a base of 34.5 percent). It increased the number of ED visits over about a year and a half by about 40 percent (0.41 visits, relative to a base of 1.02)
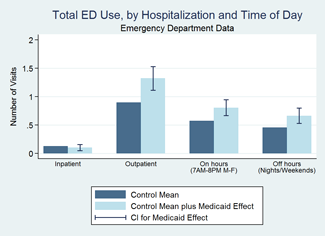
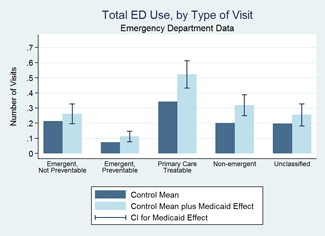
Medicaid increased visits occurring during both standard hours (weekdays) and outside of standard hours (weekends and evenings) by over 40 percent. It increased ED visits classified as "non-emergent," "primary care treatable," and "emergent, preventable." We found no statistically significant change in the use of visits classified as "emergent, non preventable." It increased outpatient emergency department visits (visits that did not result in a hospital admission), but we found no statistically significant increase in ED visits that did result in a hospital admission.
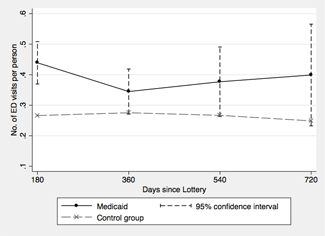
- Examining how patterns of ED use evolved over the first 2 years of coverage, we found that the increase driven by Medicaid persisted across the period. We also found no evidence that Medicaid caused new enrollees to substitute office visits for ED visits; if anything, Medicaid made them more likely to use both.
Estimated Effect of Medicaid Coverage on ED Use over Time.
Outpatient Care
- Respondents reported that coverage increased the number of office visits in the prior year by 2.7 visits, or about 50% relative to the control group average of 5.5 office visits per year. Coverage also increased the total number of prescription drugs used by recipients by .35, relative to a control group average of 2.3. (New England Journal of Medicine, 2013.)
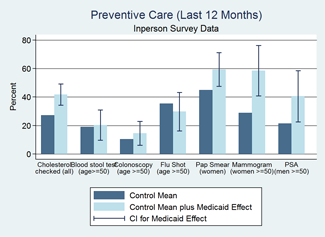
- Respondents reported substantial increases in several types of preventive care, including an increase in cholesterol monitoring of 50 percent and a doubling of mammograms.
Source: New England Journal of Medicine, 2013
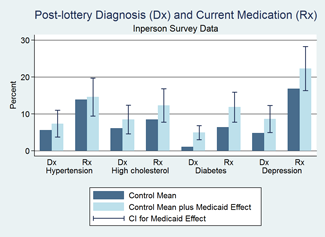
Diagnosis and Medication
- Respondents reported that Medicaid increased the probability of being diagnosed with diabetes after the lottery (by 3.8 percentage points, relative to a base rate of 1.1) and use of diabetes medication (by 5.4 percentage points, relative to a base rate of 6.4); increased the rate of diagnosis of depression (by 3.8 percentage points, relative to a base of 4.8); but had no statistically significant effect on diagnosis of or medication for hypercholesterolemia or hypertension.
Source: New England Journal of Medicine, 2013
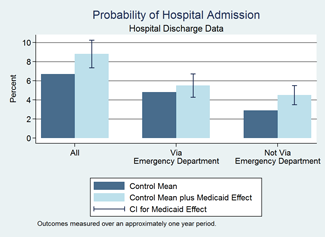
Hospitalizations
- Using state-wide hospital discharge records, we found that Medicaid increased the likelihood of being admitted to the hospital by 30 percent, driven by hospital admissions not originating in the emergency department.
Source: Quarterly Journal of Economics, 2012
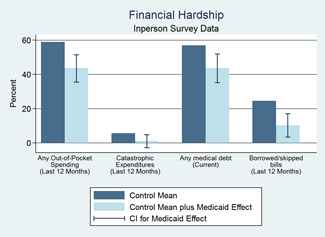
Financial Hardship
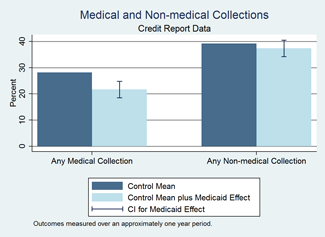
Using commercial credit reports and surveys, we found that Medicaid reduced the financial hardship of medical care for recipients.
- Respondents reported that Medicaid virtually eliminated out-of-pocket catastrophic medical expenditures and reduced the probability of having to borrow money or skip paying other bills because of medical expenses by more than 50%.
- Credit reports showed that Medicaid decreased the probability of having an unpaid medical bill sent to a collection agency by 25 percent.
Health
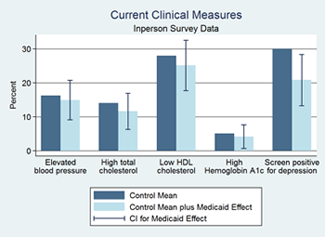
In the first one to two years of coverage, Medicaid improved self-reported health and reduced depression, but had no statistically significant effect on several measures of physical health.
- Medicaid increased the probability that people reported themselves in good to excellent health (compared with fair or poor health) by 25 percent (source: Quarterly Journal of Economics, 2012).
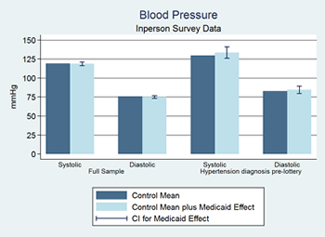
- We did not detect significant changes in measures of physical health including blood pressure (systolic or diastolic), cholesterol (HDL or total), glycated hemoglobin, or a measure of 10-year cardiovascular risk that combined several of these risk factors. Nor did we detect changes in populations thought to have greater likelihood of changes, such as those with prior diagnoses of high blood pressure of the portion of our population over age 50.
- We can reject, with 95% confidence, increases in systolic blood pressure larger than 1.93 mm Hg and decreases larger than 2.97 mm Hg. For diastolic blood pressure, we can reject, with 95% confidence, increases larger than 1.04 mm Hg and decreases larger than 2.65 mm Hg. The confidence intervals thus rule out some of the declines in blood pressure due to Medicaid that have been found in quasi-experimental studies (such as the 6-9mm decrease in diastolic blood pressure found in Lurie et al. (New England Journal of Medicine 1984; 1986)).
- Based on clinical trial evidence on diabetes medication, we would expect the observed increase in the use of medication for diabetes to decrease the average glycated hemoglobin level in the study population by 0.05 percentage points, which is well within our 95% confidence interval for the impact of Medicaid on the level of glycated hemoglobin.
- Rates of depression dropped by 9.2 percentage points, or a 30% reduction relative to the control group rate of 30 percent.
Source: New England Journal of Medicine, 2013
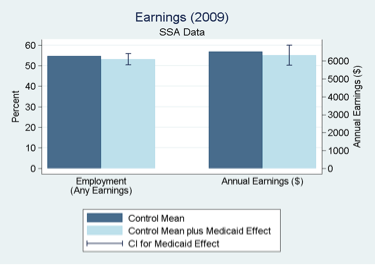
Labor Market Outcomes
Using state and federal administrative data, we found that Medicaid coverage had no statistically significant effect on labor market outcomes.
- Medicaid did not significantly change employment status or earnings. Our 95 percent confidence intervals allow us to reject that Medicaid causes a decline in employment of more than 4.4 percentage points, or an increase of more than 1.2 percentage points.
Source: American Economic Review, 2014
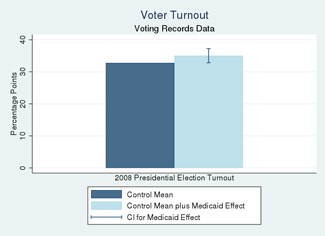
Political Participation
Using statewide voter registration and voting records data, we found that Medicaid increased voter turnout.
- Medicaid coverage increased voter turnout in the November 2008 Presidential election by about 7% overall, with the effects concentrated in men (18% increase) and in residents of Democratic counties (10% increase)
- There is no evidence of an increase in voter turnout in subsequent elections, up to and including the November 2010 midterm election.
Source: Quarterly Journal of Political Science, 2019
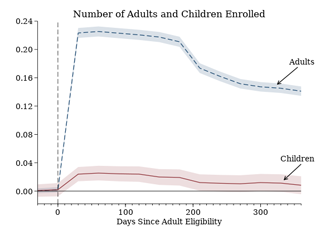
Enrollment Spillovers
Using state administrative data on Medicaid enrollment, we found statistically significant but modest and transitory impacts of adult lottery selection on children’s Medicaid enrollment.
- For every 9 adults who enroll in Medicaid due to the lottery, one additional child also enrolls at the same time.
- Both the direct effect on adult enrollment and the spillover effect on children’s enrollment fade over the subsequent year.