Increased Medicaid Reimbursement Rates Expand Access to Care
Medicaid recipients are known to experience lower access to care than privately insured patients. Potential explanations for the difficulties faced by Medicaid recipients in accessing care include their more complex medical needs, low Medicaid reimbursement rates, payment delays, or other difficulties with the Medicaid billing process. In The Impacts of Physician Payments on Patient Access, Use, and Health (NBER Working Paper 26095), researchers Diane Alexander and Molly Schnell present evidence that reimbursement rates are an important determinant of access to care, health care utilization, and health status among Medicaid recipients.
Each $10 increase in Medicaid reimbursement per visit generated a 0.3 percentage point increase in the probability that a Medicaid recipient reported a doctor visit in the past two weeks.
States have historically set their own Medicaid reimbursement rates, and those rates have varied widely. For instance, the reimbursement rate for a new patient office visit of mid-level complexity in 2009 ranged from $37 in Minnesota to $160 in Alaska. This dramatic geographic dispersion in reimbursement rates, however, was substantially reduced in 2013 by a federal mandate that required Medicaid reimbursement rates for certain primary care services to match Medicare rates. As a result, average Medicaid payments for these services rose by 60 percent, but there was substantial variation across states in the magnitude of the payment increase. For example, rates were unaffected in two states, while more than doubling in 11 other states.
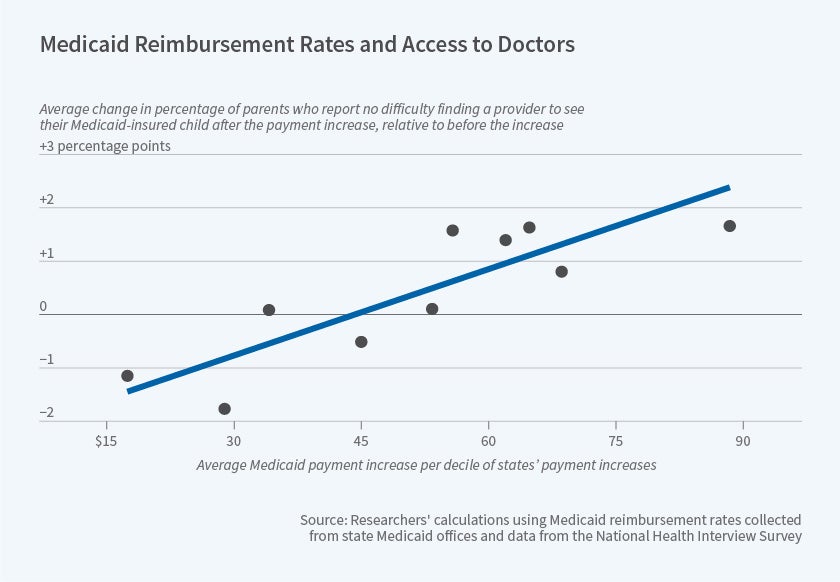
The researchers study this variation in the magnitude of the reimbursement rate change, using data from the National Health Interview Survey, and find that the policy change expanded access to care. The figure shows that, for every $10 increase in Medicaid reimbursement per visit, parents were 0.5 percentage points more likely to report no difficulty finding a provider for their Medicaid-insured children, a 25 percent change relative to the mean. Similarly, adult recipients were less likely to report being told that a physician was not accepting new patients or did not accept their insurance coverage.
This increase in access translated into a rise in health care utilization and improved health outcomes. Each $10 increase in Medicaid reimbursement per visit generated a 0.3 percentage point, or 1.4 percent, increase in the probability that a Medicaid recipient reported a doctor visit in the past two weeks and a 0.6 percentage point, or 1.1 percent, increase in the probability that a recipient reported very good or excellent health. In addition, the same $10 increase in payment per visit reduced reported school absences among primary school-aged Medicaid recipients by 14 percent, a finding that the researchers corroborate using administrative data from the National Assessment of Educational Progress.
If physicians face capacity constraints, an increase in care for Medicaid patients would imply a decline in care to other patients. However, the researchers find little evidence that Medicaid reimbursement changes had any offsetting impact on privately insured individuals, suggesting that providers had scope to increase the number of patients they saw.
Since the reimbursement mandate expired after 2015, the researchers were able to use the “reverse experiment” — when reimbursement rates reverted to their 2012 levels in most states — to validate their results.
Overall, their findings imply that changing financial incentives for providers could play an important role in improving access to care for Medicaid recipients. The researchers conclude that, when it comes to primary care office visits, “closing the gap between private insurance and Medicaid — a $45 increase in Medicaid payments for the median state — would close over two-thirds of disparities in access for adults and would eliminate such disparities among children.”
— Robin McKnight