Program Report: The Economics of Aging, 2022
When the NBER’s Program on the Economics of Aging began in 1986 under the direction of David Wise, the baby-boom generation was between the ages of 22 and 40. Long-run projections at the time forecast that the United States would transition to an older population distribution. Today, with baby boomers ranging in age from 58 to 76, that projected future is the ongoing reality of our nation. One-fifth of the population will be age 65 or older in the next decade.
Since its inception, the Economics of Aging Program’s underlying focus has been the study of the health and financial well-being of people as they age and the larger implications of a population that is increasingly composed of older people. The program continues this broad focus as new and ongoing challenges emerge and evolve.
To illustrate the wide and multidisciplinary scope of research by program affiliates, I briefly describe ongoing work in four areas: the widening health disparities across education and region, a rising number of patients and caregivers struggling with Alzheimer’s disease, the impact of the COVID-19 pandemic on the elderly, and the continuing evolution of the financial, physical, and mental health of retirees. This review is only a partial summary of the wide-ranging research carried out by program affiliates. Since the last program report, in 2014, more than 600 working papers related to the Economics of Aging Program have been distributed. Researchers have also published dozens of studies on aging in scientific and clinical journals, precluding inclusion in the NBER Working Paper series.
Widening Inequality in Mortality by Education and Place
Research by Anne Case and Angus Deaton illustrates the far-reaching effects of “deaths of despair” arising from drug overdoses, suicide, and alcoholism, and the very close association of these deaths with education.1 These deaths have not only continued to rise, but have largely been among those without a four-year college degree — the majority of American adults.2 As a consequence, mortality in the US is falling for the college-educated and rising for those without a degree — something not seen in other rich countries. One explanation for this US exceptionalism is the health-care system and the associated approach to financing health care. Another contributor is the drug epidemic and the explosion of prescription opioids after 1996, followed by an epidemic of illegal drug use, including use of diverted prescription drugs, heroin, and fentanyl. Abby Alpert, William Evans, Ethan Lieber, and David Powell find that the introduction and marketing of OxyContin explain a substantial share of overdose deaths over the last two decades.3
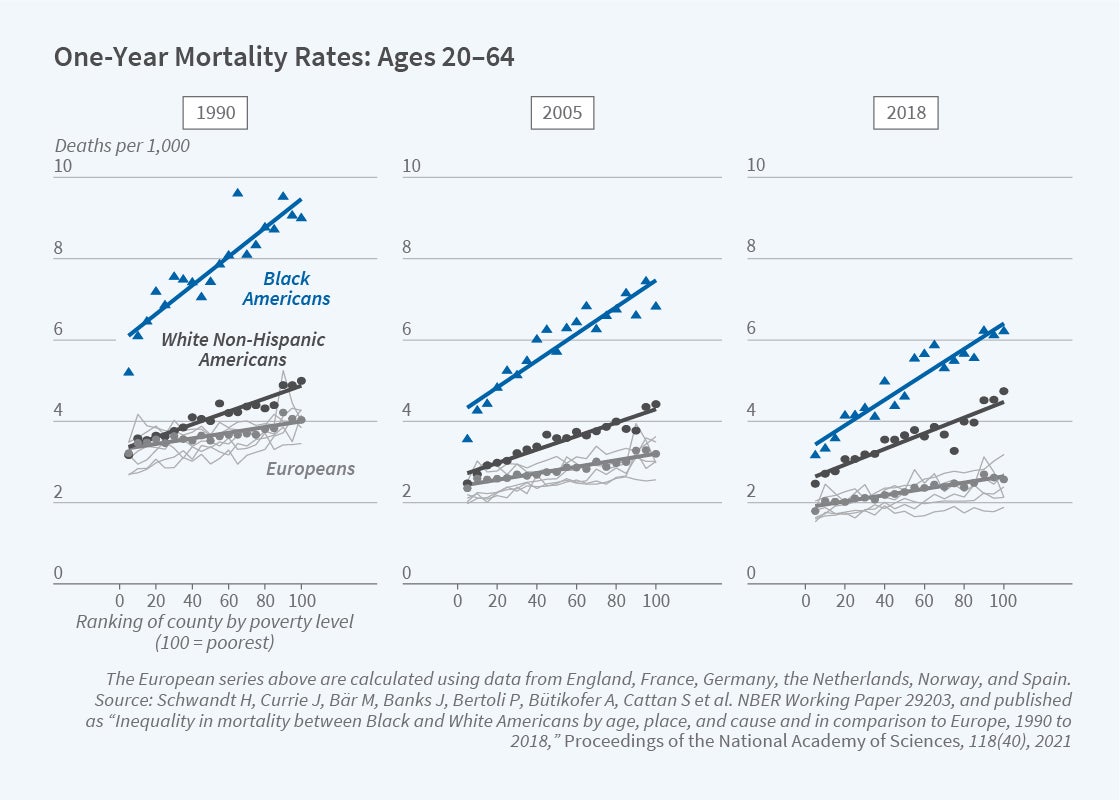
Hannes Schwandt, Janet Currie, and a team of research collaborators drawn from many nations analyze mortality rates in the US and other high-income countries. They compare high-income and low-income regions in the US with similarly high- and low-income regions in nine European countries. This enables them to estimate separately the income gradient of mortality by country; in the US they estimate separate gradients for Blacks and Whites of all ages.4 While in 1990 White Americans and Europeans in rich areas had similar overall life expectancy, since then even rich White Americans have lost ground relative to Europeans. As shown in Figure 1, on the next page, there was a reduction in the midlife life expectancy gap between Black Americans and Europeans, but life expectancy for both Black and White Americans plateaued or slightly declined after 2012. The comparison with European countries suggests that substantial improvements in mortality rates of both Black and White Americans are still feasible in both high-income and low-income areas.
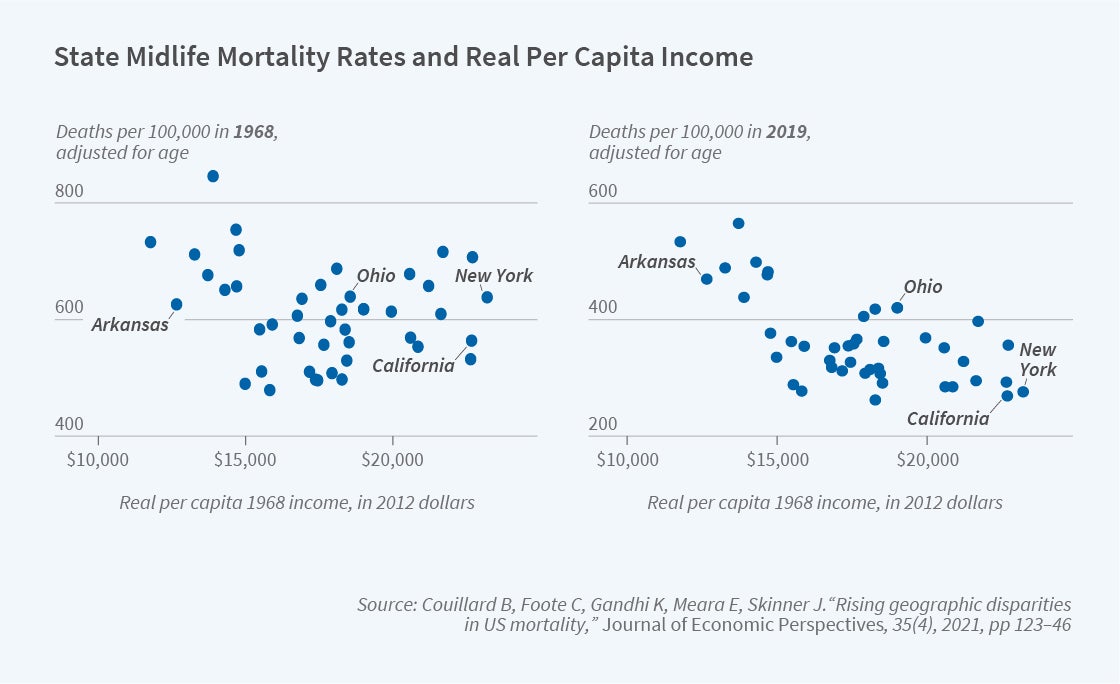
There are widening geographic disparities in mortality within the US. Benjamin Couillard, Christopher Foote, Kavish Gandhi, Ellen Meara, and I find that geographic inequality in mortality for midlife Americans increased by about 60 percent between 1992 and 2016.5 This was not simply because states like New York or California benefited from having a high fraction of college-educated residents who enjoyed the largest health gains during the last several decades. Nor was higher dispersion in mortality caused entirely by the increasing importance of deaths of despair or by rising regional income inequality during the same period. Instead, over time, state-level mortality has become increasingly correlated with state-level income. In 1992, income explained only 3 percent of mortality inequality, but by 2016 state-level income explained 58 percent. Figure 2 illustrates this growing association. These mortality patterns are consistent with high-income states during the twentieth century being better able to enact public health strategies and adopt behaviors that, over the next quarter century, resulted in pronounced relative declines in mortality in some but not all states.
The role of place — the set of health factors associated with one’s state, city, or town — has also been a topic of ongoing research. Remarkably, “place” seems to matter even when people aged 65 or older move. Tatyana Deryugina and David Molitor follow Medicare cohorts living in New Orleans to study the long-run effects of Hurricane Katrina.6 They find that even after including the storm’s initial effects on mortality, the hurricane improved eight-year survival by 2.07 percentage points, with migration to lower-mortality regions explaining most of this increase. Migrants’ mortality is lower in destinations with healthier behaviors and higher incomes; the quality and quantity of health care in a locality appears unimportant.
One advantage of studying those who move is that most individuals’ health does not change much around the time of the move, so it allows for a reliable estimate of the influence of place on health. Amy Finkelstein, Matthew Gentzkow, and Heidi Williams study Medicare movers at the national level and find substantial effects of current location. Moving from a 10th to a 90th percentile location is predicted to increase life expectancy at age 65 by 1.1 years.7 Places with favorable life expectancy are associated with higher quality and quantity of health care, less extreme climates, lower crime rates, and higher socioeconomic status.
Alzheimer’s Disease, Cognition, and Aging
With support from the National Institute on Aging, research by program affiliates has increasingly focused on the economic and behavioral consequences of Alzheimer’s disease, which affects approximately one in 10 people aged 65 or older and is the most costly disease in the United States. Alzheimer’s is a central concern for patients, caregivers, and healthcare policymakers. Amitabh Chandra, Courtney Coile, and Corina Mommaerts emphasize the defining features of the economics of the disease, including the challenges of choices by cognitively impaired patients that affect their health and financial well-being and the potential importance of dynamic contracts between patients and caregivers that are difficult to enforce.8 They suggest high returns to focusing on innovation in Alzheimer’s prevention, treatment, and care, given the enormous social cost and present lack of understanding of its causes.
While much of the research on Alzheimer’s has focused on the costs of the late-stage disease, emerging research suggests an important impact of cognition more generally — even prior to diagnosis — on financial health. For example, John Ameriks, Andrew Caplin, Minjoon Lee, Matthew Shapiro, and Christopher Tonetti find that cognitive decline, often unnoticed, can delay the transfer of control over financial matters to someone else in the family, often with important adverse effects on financial well-being.9
Other research has focused on factors that can potentially increase the likelihood of Alzheimer’s later in life. Kelly Bishop, Jonathan Ketcham, and Nicolai Kuminoff find that long-term exposure to fine-particulate air pollution (PM2.5) increases the risk of developing Alzheimer’s disease and related dementias.10 Using the expansion of the Clean Air Act as a shock to the level of fine particulates, they find relatively large effects of reducing PM2.5 rates. They estimate that federal regulations associated with the Clean Air Act led to nearly 182,000 fewer people with dementia.
The Impact of COVID-19 on Older Americans
It is well understood that COVID-19 led to more than one million lives lost, but it is difficult to measure all deaths that were a consequence of the pandemic, not just deaths caused by the virus. To answer the broader question, Christopher Ruhm analyzes death data from March 2009 through February 2021. He estimates that there were nearly 700,000 excess deaths during the first year of the pandemic, with 83 percent of these attributed directly to COVID-19 and the remainder arising from cardiovascular deaths, motor vehicle accidents, drug overdoses, and homicides.11
Marcella Alsan, Chandra, and Kosali Simon document the dramatic inequality associated with the health shocks of the early pandemic.12 They find that in 2020, Hispanic and Black Americans experienced 39.5 and 25 percent increases respectively in excess mortality relative to trend, compared to a less than 15 percent increase for Whites. Losses in potential years of life were three to four times larger among Hispanics and Blacks than among Whites. Individual-level data from a commercially insured population show that otherwise similar Black and Hispanic enrollees were hospitalized due to COVID-19 at a higher rate than White enrollees. Lauren Gilstrap, Weiping Zhou, Alsan, Anoop Nanda, and I also find higher excess mortality for Medicare enrollees age 65 or older. Mortality rose 26 percent for people with Alzheimer’s disease and related dementias (ADRD) in 2020 compared to 2019; this contrasts with an increase of just 12 percent for a comparably aged group without ADRD.13 In regions with little reported COVID-19 during the pandemic’s early months, mortality declined 2 percent for those without ADRD but increased 6 percent for people with ADRD. Christopher Cronin and Evans offer a potential explanation for this puzzling finding. They discover that mortality rates rose in low-COVID-19 regions for high-quality nursing homes, whose lockdowns were effective in reducing the spread of COVID-19 but may have also increased non-COVID-19 mortality. This may have been particularly true for ADRD patients, who comprise a large fraction of nursing home residents, because their normal caregivers may not have been available.14
Relatively little is currently known about educational differences in mortality during the pandemic. Because those without a college degree are likely to have been exposed disproportionately to COVID-19 through employment, one might have expected the education mortality gap to have widened since 2019. However, Case and Deaton find that mortality rates increased in 2020 over 2019 in roughly equal proportions for those with and without a college degree, irrespective of age, sex, or race/ethnicity.15 A college degree was strongly associated with a longer life span before the COVID-19 pandemic, and it continued to be protective in the first wave of the pandemic as well.
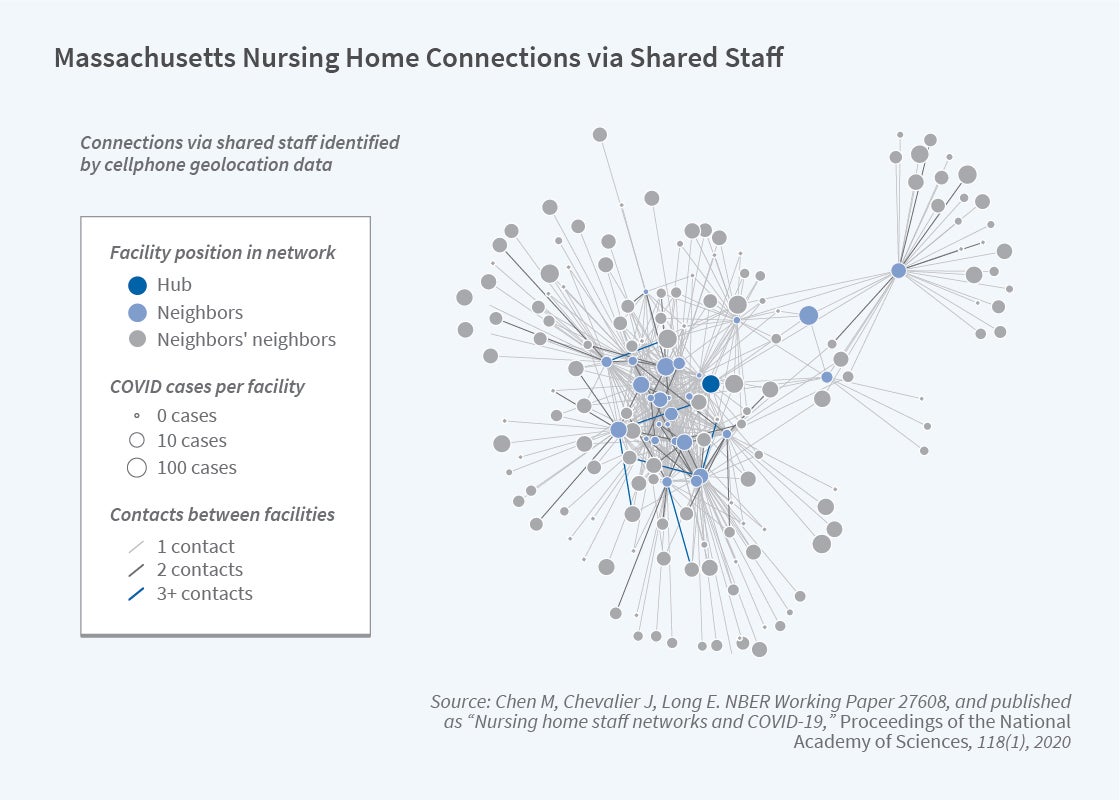
It is well known that nursing homes were hit hard in the first year of the pandemic, but why is less clear. Was it simply because nursing home patients were older and more susceptible, or were there other factors that elevated nursing home mortality? Using novel approaches relying on data from more than 30 million US smartphones, M. Keith Chen, Judith Chevalier, and Elisa Long find that nursing homes with staff working at multiple facilities were more likely to experience outbreaks of COVID-19 than those without such links.16 They track 510,000 phones that were observed to have been in at least one nursing home over the six-week period after March 13, when a nationwide lockdown on nursing homes went into effect; about 7 percent were observed in at least two facilities. Homes with no documented cases of COVID-19 had an average of 11.8 connections to other homes, where a connection means a cellphone observed at that home was also observed in another home. By comparison, homes with confirmed or suspected COVID-19 cases averaged 17.3 connections. The researchers estimate that eliminating staff overlap among nursing homes could have reduced coronavirus cases in nursing homes by as much as 44 percent.
Financial, Mental, and Physical Well-Being during Retirement
Researchers have studied the shift from defined benefit to defined contribution retirement plans and the impact of this shift on retirement security and preretirement behavior. Recent research finds that large groups of Americans have been left behind by this shift. For example, Kai Yuan Kuan, Mark Cullen, and Sepideh Modrek examine 401(k) saving behavior of continuously employed workers over an eight-year period at a single, geographically diverse employer. They find that both Black and Hispanic employees are less likely to participate in the 401(k) plan, and that conditional on participation, Black employees contribute a lower proportion of their income to their 401(k) plan on average, tend to draw down their 401(k) balances more often, and favor safer assets within their plan options.17 These combined effects have a large impact on 401(k) balances and hence overall wealth accumulation.
Financial literacy — having a basic understanding of aspects of investing such as the power of compound interest — also impacts wealth accumulation. Marco Angrisani, Jeremy Burke, Annamaria Lusardi, and Gary Mottola find that financial literacy has significant predictive power for future financial outcomes, even after controlling for baseline outcomes and a wide set of demographics and individual characteristics that influence financial decision-making.18
There are clear racial and ethnic disparities in wealth accumulation. Research has also explored differences in earnings and work capacity. Benjamin Berger, Italo Lopez Garcia, Nicole Maestas, and Kathleen Mullen study how functional abilities and potential earnings evolve as individuals age.19 They find that average functional abilities and potential earnings decline only slightly with age, and that work capacity differences by race, ethnicity, and gender are small. These results imply that health is not a major driver of observed earnings disparities. The researchers find, however, that gaps in work capacity by education are large and increase with age.
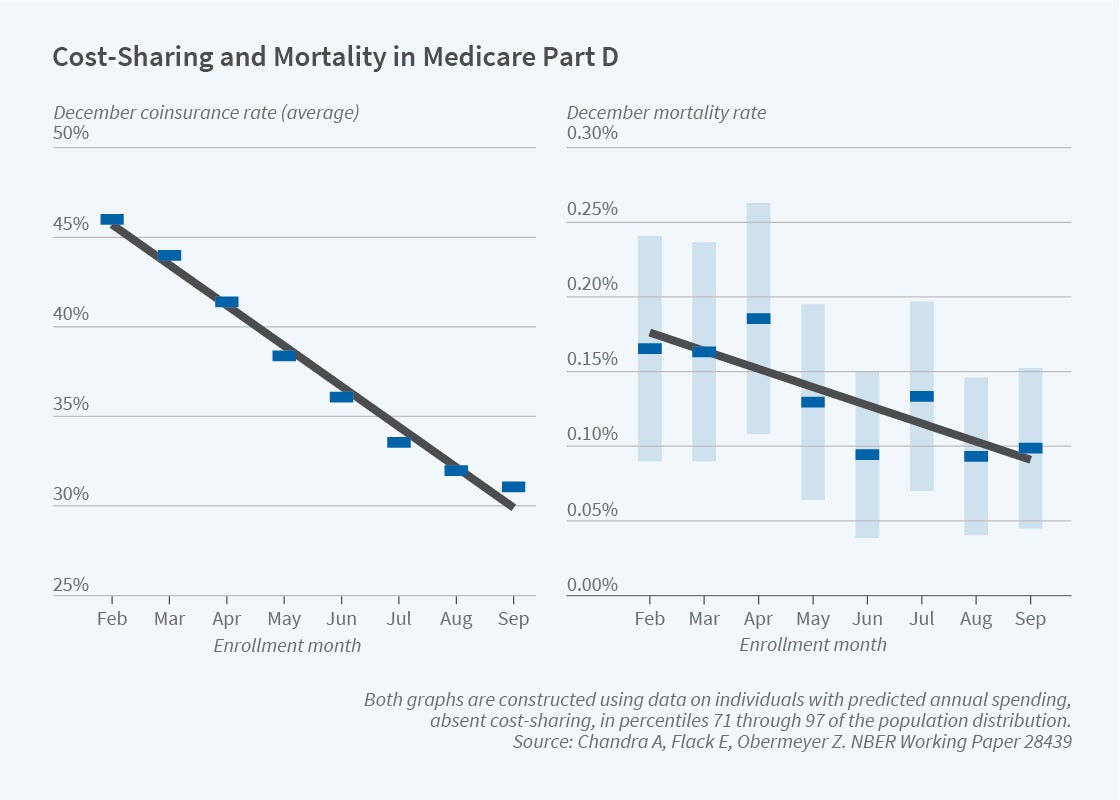
Program affiliates have not only analyzed how government incentives affect financial preparedness for retirement, but also how government programs affect the health of retirees. For example, Chandra, Evan Flack, and Ziad Obermeyer examine Medicare’s prescription drug benefit program and find that an increase of approximately $10.40 in out-of-pocket costs per drug prescription leads to a 23 percent drop in total drug consumption and a 33 percent increase in monthly mortality.20 The mortality effect appears to be the consequence of cutbacks in life-saving medicines like statins and antihypertensives, for which clinical trials show large mortality benefits.
The researchers use the month during which Medicare enrollees become eligible for Medicare Part D as a natural randomization for whether they fall into a gap in coverage, which typically occurs after spending $2,500 on prescription drugs. People who turn 65 later in the year are less likely to end up in the coverage gap simply because they experience fewer months of Part D spending. The first panel in Figure 4 shows this; by December, coinsurance rates are highest for those born in February and fall by an average of 2.3 percentage points in each subsequent enrollment month. The second panel of Figure 4 shows a similar pattern for mortality rates in this group. On average, each month of later enrollment reduces December mortality by 0.0113 percentage points, a 9 percent decrease. The findings suggest that enrollees respond to incentives regarding coinsurance for drug purchases, but do so in ways that may have unintended private and social costs.
Endnotes
Deaths of Despair and the Future of Capitalism, Case A, Deaton A. Princeton, NJ: Princeton University Press, 2020.
“The Great Divide: Education, Despair and Death,” Case A, Deaton A. NBER Working Paper 29241, September 2021. Forthcoming in the Annual Review of Economics 14, August 2022.
“Origins of the Opioid Crisis and Its Enduring Impacts,” Alpert A, Evans W, Lieber E, Powell D. NBER Working Paper 26500, November 2019, and The Quarterly Journal of Economics 137(2), May 2022, pp. 1139–1179.
“Inequality in Mortality between Black and White Americans by Age, Place, and Cause, and in Comparison to Europe, 1990–2018,” Schwandt H, Currie J, Bär M, Banks J, Bertoli P, Bütikofer A, Cattan S, et al. NBER Working Paper 29203, September 2021, and Proceedings of the National Academy of Sciences 118(40), September 2021.
“Rising Geographic Disparities in US Mortality,” Couillard B, Foote C, Gandhi K, Meara E, Skinner J. Journal of Economic Perspectives 35(4), Fall 2021, pp. 123–146.
“Does When You Die Depend on Where You Live? Evidence from Hurricane Katrina,” Deryugina T, Molitor D. NBER Working Paper 24822, revised December 2019, and American Economic Review 110(11), November 2020, pp. 3602–3633.
“Place-Based Drivers of Mortality: Evidence from Migration,” Finkelstein A, Gentzkow M, Williams H. NBER Working Paper 25975, June 2019, and American Economic Review 111(8), August 2021, pp. 2697–2735.
“What Can Economics Say about Alzheimer’s Disease?” Chandra A, Coile C, Mommaerts C. NBER Working Paper 27760, July 2021. Forthcoming in the Journal of Economic Literature.
“Cognitive Decline, Limited Awareness, Imperfect Agency, and Financial Well-Being,” Ameriks J, Caplin A, Lee M, Shapiro M, Tonetti C. NBER Working Paper 29634, January 2022.
“Hazed and Confused: The Effect of Air Pollution on Dementia,” Bishop K, Ketcham J, Kuminoff N. NBER Working Paper 24970, revised August 2019.
“Excess Deaths in the United States during the First Year of COVID-19,” Ruhm C. NBER Working Paper 29503, November 2021.
“The Great Unequalizer: Initial Health Effects of COVID-19 in the United States,” Alsan M, Chandra A, Simon K. NBER Working Paper 28958, June 2021, and Journal of Economic Perspectives 35(3), Summer 2021, pp. 25–46.
“Trends in Mortality Rates among Medicare Enrollees with Alzheimer’s Disease and Related Dementias before and during the Early Phase of the COVID-19 Pandemic,” Gilstrap L, Zhou W, Alsan M, Nanda A, Skinner J. JAMA Neurology 79(4), April 2022, pp. 342–348.
“Nursing Home Quality, COVID-19 Deaths, and Excess Mortality,” Cronin C, Evans W. NBER Working Paper 28012, October 2020, and Journal of Health Economics 82, March 2022, article 102592.
“Mortality Rates by College Degree before and during COVID-19,” Case A, Deaton A. NBER Working Paper 29328, revised October 2021.
“Nursing Home Staff Networks and COVID-19,” Chen M, Chevalier J, Long E. NBER Working Paper 27608, revised October 2020, and Proceedings of the National Academy of Sciences 118(1), December 2020, e2015455118.
“Racial Disparities in Savings Behavior for a Continuously Employed Cohort,” Kuan K, Cullen M, Modrek S. NBER Working Paper 20937, February 2015.
“The Stability and Predictive Power of Financial Literacy: Evidence from Longitudinal Data,” Angrisani M, Burke J, Lusardi A, Mottola G. NBER Working Paper 28125, November 2020.
“The Link between Health and Working Longer: Disparities in Work Capacity,” Berger B, Lopez Garcia I, Maestas N, Mullen K. NBER Working Paper 30036, May 2022.
“The Health Costs of Cost-Sharing,” Chandra A, Flack E, Obermeyer Z. NBER Working Paper 28439, February 2021.


