The Effects of Employee Vaccine Mandates in Nursing Homes
During the COVID-19 pandemic, nursing home residents were particularly vulnerable due to their age and preexisting health conditions. In 2020, nearly 20 percent of COVID-19 cases in nursing homes resulted in death. The vast majority of nursing home residents were fully vaccinated within six months of the vaccine’s release in December 2020, but vaccination rates for staff lagged behind, with less than half of certified nursing assistants (CNAs) — who constitute the majority of nursing home employees — vaccinated over the same period.
In an effort to protect vulnerable patients, many nursing homes considered requiring all employees to be vaccinated. But they faced a difficult trade-off. A mandate could potentially improve health outcomes by reducing transmission, but it could also lower the quality of care by increasing staff turnover.
In The Health and Employment Effects of Employer Vaccination Mandates (NBER Working Paper 33072), researchers Ashvin Gandhi, Ian Larkin, Brian McGarry, Katherine Wen, Huizi Yu, Sarah Berry, Vincent Mor, Maggie Syme, and Elizabeth White evaluate this trade-off. They compare changes in employment and health outcomes at facilities that adopted mandates before September 2021 to changes in outcomes at facilities that did not. Their study brings together daily data from the Centers for Medicare and Medicaid Services on staffing and weekly data from the CDC’s National Healthcare Safety Network on COVID-19 transmission and mortality.
Nursing homes that mandated vaccination for all staff members experienced fewer COVID-19 deaths and only a modest increase in staff turnover.
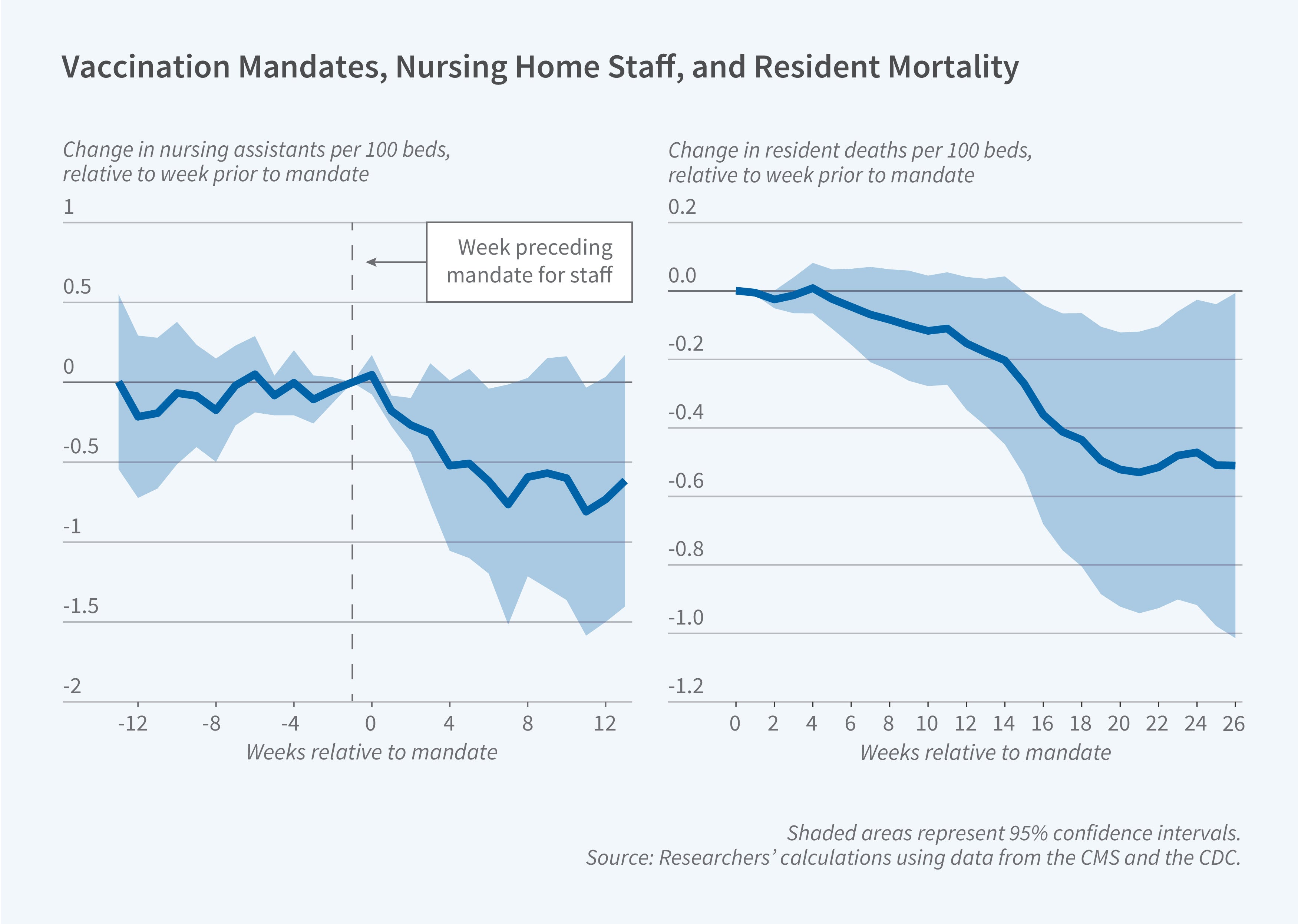
Vaccine mandates reduced the number of CNAs employed at the typical 100-bed facility by 0.73 (4 percent), with reductions concentrated among part-time workers. The decreased number of employees resulted in a reduction of two minutes of staffing per patient-day (a 1 percent decline). This modest reduction in staffing was associated with only limited indications of worsening quality of care. Most indicators, such as the number of patient falls, pressure ulcers, and urinary tract infections, were unaffected.
At the same time, mandates increased staff vaccination rates by 13 percentage points relative to rates at facilities without mandates, where on average about 65 percent of the staff were vaccinated. Mandates substantially reduced infection rates for staff and for residents. In the 26 weeks after a mandate was announced, there were 4.4 fewer resident COVID-19 cases per 100 beds (a 61 percent decline) and 0.5 fewer resident deaths per 100 beds (a 65 percent decline).
The researchers conclude that vaccine mandates saved one patient life for every two facilities that enacted a mandate. If all US nursing homes had adopted vaccine mandates in December 2020, nearly 10,000 patient lives could have been saved. Because facilities in higher-income areas were more likely to adopt vaccine mandates, the benefits of the mandates that were adopted were concentrated among patients who were higher income, White, and lived in suburban and rural areas.
— Robin McKnight
The researchers acknowledge support from the National Institute on Aging (U54AG063546).


