Reductions in Mortality Rates and Health Disparities with the Introduction of Penicillin
The discovery of penicillin was arguably one of the most important medical advances of the 20th century. In Technological Progress and Health Convergence: The Case of Penicillin in Post War Italy (NBER Working Paper 25541), researchers Marcella Alsan, Vincenzo Atella, Jay Bhattacharya, Valentina Conti, Iván Mejía-Guevara and Grant Miller assess the distributional impact of this innovation on mortality in Italy following World War II.
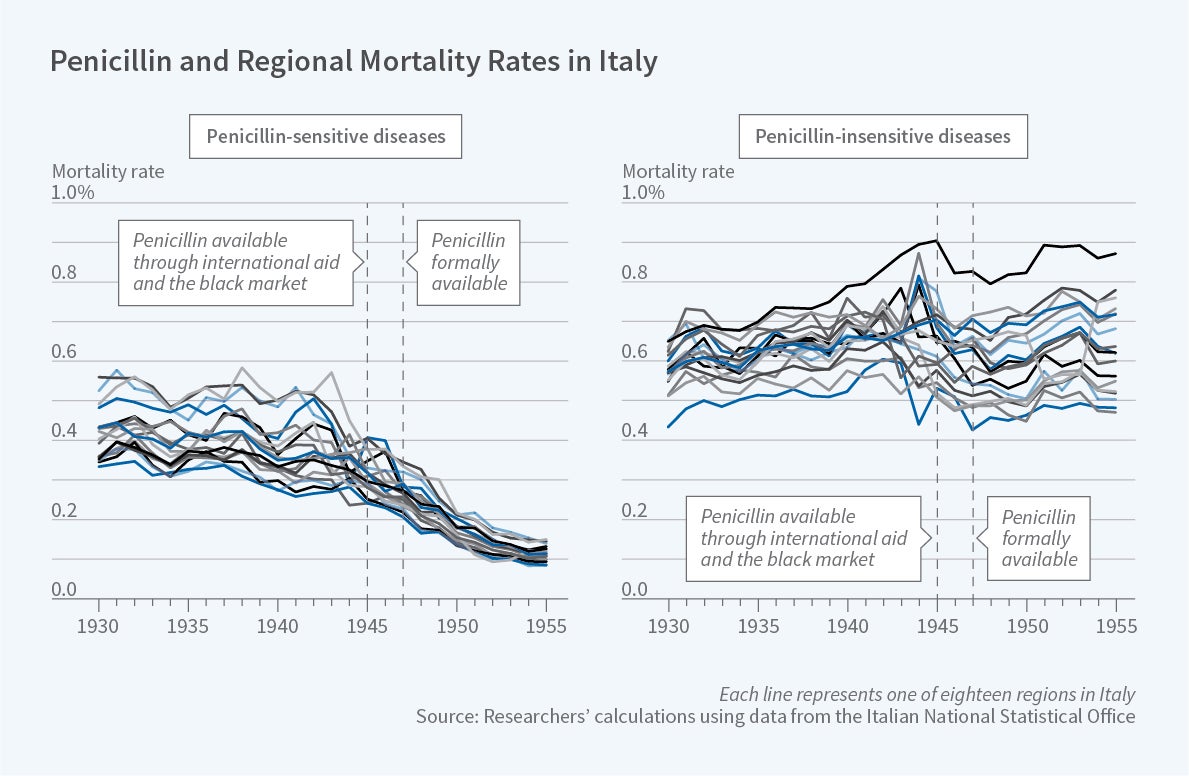
While there were long-standing regional disparities in penicillin-sensitive mortality rates in Italy prior to 1947, these regional mortality rates quickly converged following penicillin’s introduction.
Penicillin was available in Italy in the mid-1940s in only limited quantities through international aid and the black market. Beginning with its official introduction in 1947, however, it became widely accessible, at no out-of-pocket cost, to any patient with a physician’s prescription. The researchers rely on this discrete change in the availability of penicillin to provide evidence about its impact on mortality convergence across regions of Italy.
Using newly-digitized Italian Vital Statistics data, the researchers show that the mortality rates for penicillin-sensitive causes of death – such as pneumonia, scarlet fever, and syphilis – fell sharply beginning in 1947. By contrast, mortality rates for penicillin-insensitive causes of death – such as influenza, cancer and heart disease – exhibited no apparent changes at that time. The researchers estimate that mortality for penicillin-sensitive causes of death fell by 0.3 per thousand following the introduction of penicillin, a 58 percent decline relative to the mean prior to 1947.
Furthermore, using a variety of econometric and demographic techniques, the researchers find evidence of mortality rate convergence across regions of Italy. While there were long-standing regional disparities in penicillin-sensitive mortality rates in Italy prior to 1947, these regional mortality rates quickly converged following penicillin’s introduction. In contrast, the disparities in mortality from other causes did not. Relative to years prior to 1947, the introduction of penicillin reduced the dispersion of penicillin-sensitive mortality rates across regions by 68 percent, explaining 40 percent of all-cause convergence over this period.
One factor that could confound this analysis is the conclusion of World War II shortly before the introduction of penicillin in Italy. Because infectious disease mortality tends to increase during wars, the authors consider this alternative explanation for their results. They estimate models separately for regions that experienced higher vs. lower degrees of exposure to the war, and find that the mortality reductions were slightly — but statistically significantly — higher in the areas with less exposure to the war.
In addition, they find that their results are statistically unaffected if they exclude the years of greatest conflict intensity in Italy — 1943 to 1945 — from their sample period. These patterns suggest that the overall results are unlikely driven by the conclusion of the war. The researchers also find that competing risks are unlikely to explain the results, since even limiting to a short period of time after the introduction of penicillin, the estimated differences are still large.
The researchers note that, in general, new medical technologies have the potential to either reduce or exacerbate health disparities, depending on whether they are disproportionately available to the elite. In the case of penicillin, the evidence suggests that the technological advance acted to reduce disparities in postwar Italy.
— Robin McKnight
The researchers acknowledge funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) through grant 5K01-HD084709 and the National Institute on Aging (NIA) through grant 5P30AG017253.