Higher Medicare Advantage Enrollment Reduces Opioid Use
The public health costs of opioid abuse have continued to climb in the United States, contributing to recent declines in life expectancy. One response to mitigating this public health crisis has been to try to reduce use — and especially misuse — of prescription opioids. In The Effects of Medicare Advantage on Opioid Use (NBER Working Paper 25327), Laurence C. Baker, Kate Bundorf and Daniel Kessler suggest that insurance design could contribute to these efforts.
Medicare Advantage enrollment causes a 37 percent reduction in the probability of receiving an opioid prescription.
The researchers ask whether insurance design — specifically, the integration of prescription drug benefits with other medical benefits — can play a role in decreasing the number of opioid prescriptions. To answer this question, they focus on Medicare prescription drug coverage. Medicare is the largest purchaser of opioids in the US, accounting for about a quarter of all opioid prescriptions.
Medicare enrollees can choose to receive prescription drug insurance from a stand-alone Part D plan or through a Medicare Advantage (MA) plan that integrates insurance coverage for prescription drugs with coverage for other medical care. The researchers point out that MA insurers have the incentive to reduce any prescription opioid use that generates offsetting increases in inpatient or outpatient costs. In contrast, stand-alone prescription drug plans do not bear the costs of other medical care obtained by their enrollees, so do not have an incentive to consider such impacts.
In addition, MA plans have greater opportunity than stand-alone Part D plans to affect opioid prescription rates. For example, MA plans can choose their network of providers. Selecting physicians on the basis of their tendency to prescribe opioids could affect opioid prescription rates among MA enrollees. Other insurer strategies, such as utilization review, could have a similar effect.
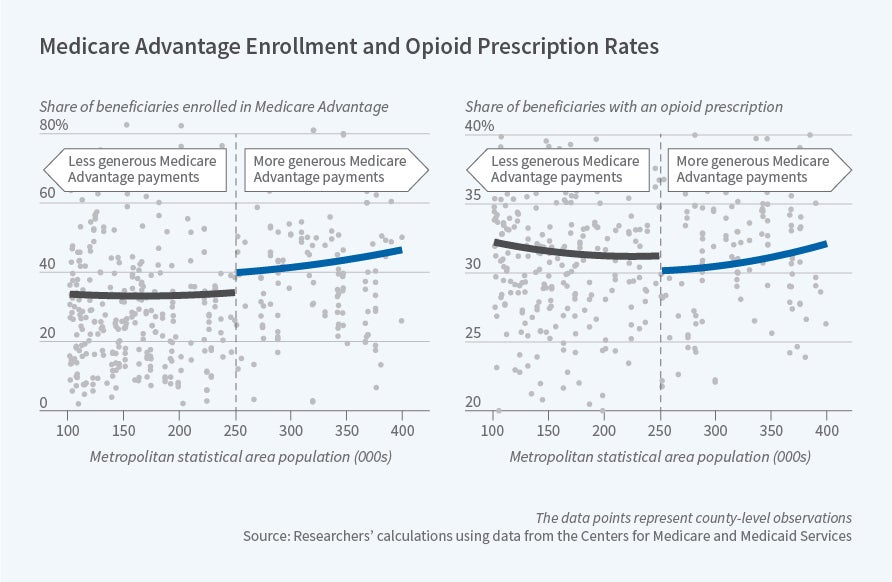
To explore the impact of MA enrollment on opioid prescription patterns, the researchers compare Medicare beneficiaries in counties that receive more generous MA payments to beneficiaries in similar counties that receive less generous payments. The government’s formula for paying Medicare Advantage plans includes minimum payment levels — or “floors” — that are intended to encourage insurer participation in the program; the payment “floor” increases discontinuously when the population of the metropolitan statistical area within a county exceeds 250,000. Consistent with prior evidence, the researchers find that beneficiaries who live in counties that receive these higher payments are 12 percentage points more likely to enroll in MA than beneficiaries in less populous counties.
The researchers find that there is a corresponding reduction in opioid prescription rates in counties that have higher MA enrollment due to the higher payments. This pattern suggests a causal relationship between MA enrollment and opioid prescription rates. The researchers conclude that MA enrollment causes a 12 percentage point reduction in the probability of receiving an opioid prescription, a 37 percent reduction relative to the average opioid prescription rate in this sample.How does Medicare Advantage reduce opioid prescriptions? The researchers suggest that one key mechanism is limiting prescriptions from high-volume prescribers of opioids. In their sample, 27 percent of opioid prescriptions are written by only 1 percent of prescribers. MA enrollees are 6 percentage points less likely to receive a prescription from one of these providers. The reduced prescriptions from these high-volume providers account for half of the overall effect of MA enrollment on opioid use.
The researchers note that their analysis cannot distinguish between appropriate and inappropriate use of prescription opioids. However, they speculate that the reduced prescriptions from high-volume providers may be an indication that MA plans are reducing inappropriate use.
Prior research suggests that MA enrollment is associated with increased use of other types of prescription drugs. The contrasting pattern for opioids, therefore, likely reflects a specific effort by insurers to reduce opioid use, rather than broader constraints on prescription drug use. The researchers conclude that their results support the idea that “integration of prescription drug coverage with the other benefits provided by Medicare Advantage plans improves the quality of care.”
— Robin McKnight