Long-Term Care Hospitals Discharge Patients Strategically
Containing costs while providing high-quality health care is a top priority for the Medicare program. Payments to hospitals are an area of particular interest, with $145 billion spent on reimbursements for inpatient stays in 2015.
Since 1983, Medicare has used a prospective payment system that reimburses hospitals a fixed amount per hospital stay based on the patient's diagnosis at admission (the "diagnosis-related group," or DRG). Such a system may incentivize hospitals to provide care efficiently, since keeping a patient in the hospital longer or providing additional services does not increase reimbursements.
Long-term care hospitals (LTCHs), which specialize in treating patients with serious medical conditions who require pro-longed care, are also reimbursed by prospective payment. As patients at LTCHs have longer stays, reimbursement rates for LTCHs are higher than those for traditional hospitals, but there is also a reduced rate for "short stay outliers" (SSOs), patients whose stay is less than a pre-specified number of days (where the exact cutoff depends on the DRG). This policy is intended to ensure that only patients who truly require long-term care are admitted to LTCHs. However, this two-tiered payment system creates the possibility that hospitals may strategically extend some patients' stays beyond the cutoff date in order to receive the higher reimbursement rate.
In Strategic Patient Discharge: The Case of Long-Term Care Hospitals (NBER Working Paper No. 22598), researchers Paul Eliason, Paul Grieco, Ryan McDevitt, and James Roberts explore this issue. The researchers use Medicare claims data from 2002-13. They focus on one particular DRG, respiratory system diagnosis with at least 96 hours of ventilator support, which is both the most common and highly reimbursed DRG. They observe over 90,000 patients with this DRG who are subsequently discharged to home or to a nursing facility.
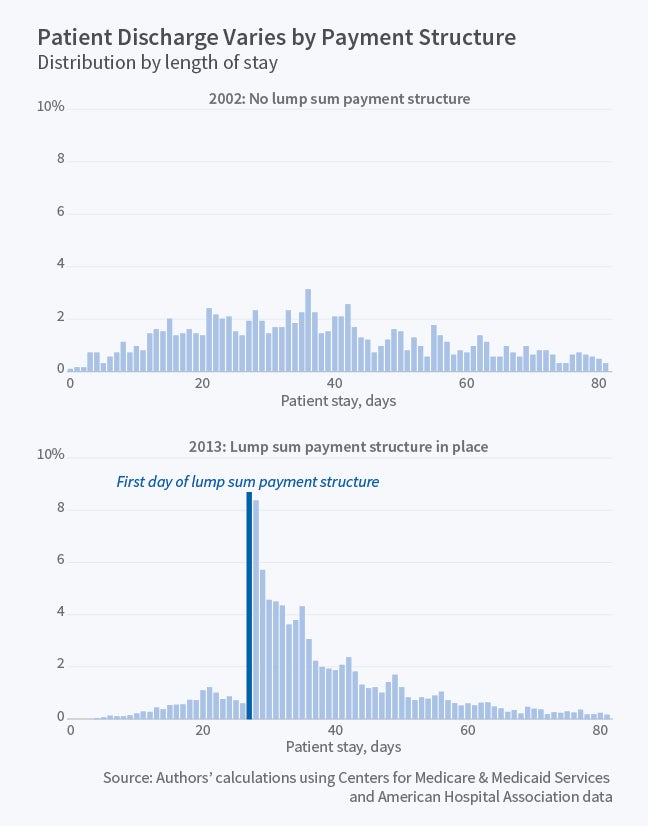
The figure shows the distribution of stay lengths for patients with this DRG in 2002, before the two-tiered payment system was introduced, and in 2013, after this system had been in place nearly a decade and when the threshold stay length for a higher reimbursement rate was 27 days. In 2002, the share of discharges occurring on any given day is fairly constant, with about 2 percent of patients discharged each day between day 10 and day 40. By contrast, in 2013 there is a sharp spike in discharges once the stay length reaches 27 days. The probability of being discharged immediately after the cutoff date is more than seven times higher than the probability of being discharged just before the cutoff, 10.2 vs. 1.4 percent. The probability remains elevated for about a week after the cutoff, while discharge rates before day 27 are much lower in 2013 than they were in 2002.
This pattern is unlikely to result from medical advances, particularly given that other DRGs experienced the same pattern of an emerging spike in discharges at their own cutoffs; as the researchers note, "it is even more unlikely that any coincident medical advances occurred in each of these different DRGs in a way that happened to shift discharges to precisely after their DRGs' SSO thresholds." They report that the spike in discharges at the cutoff date is largest when the patient is discharged to home, where the exact date of release is presumably easier to manipulate; there is no spike at the cutoff date for patients who ultimately die in the LTCH.
The researchers also examine whether the probability of strategic discharge is higher among for-profit hospitals, which may have a stronger incentive to engage in this behavior due to the profit-seeking motive. They find that the ratio of discharges on the cutoff day relative to the day before is twice as high in for-profit hospitals (9.2) as in non-profit hospitals (4.6). They also find that in LTCHs acquired by the two dominant chains, Kindred or Select, the ratio of discharges on the cutoff day relative to the day before rose from 8.7 pre-acquisition to 15.1 post-acquisition, "suggesting that target LTCHs adopt their acquirers' discharge policies." They also find that LTCHs that are co-located with general acute-care hospitals engage in this behavior more, "perhaps because they face fewer barriers for transferring patients across floors in order to maximize Medicare payments."
Finally, the researchers estimate a model of discharge behavior and use it to simulate several alternative payment policies. They project that removing the sharp increase in payments at the SSO threshold would reduce reimbursements by $18.9 million for the nine most common DRGs, as LTCHs would respond by discharging patients sooner. As the researchers conclude, "because the current reimbursement formula provides a large jump in payments for patients who stay past a certain threshold, LTCHs respond to these financial incentives by keeping patients until right after they reach this point. [These] findings suggest that LTCHs keep patients too long as a result of this payment scheme, resulting in needless costs for Medicare and an untold burden for patients."